Case Study #1: Low Back Pain
Hey Break Free Community,
I thought I’d take a break from blog writing and share common presentations I’ve seen in my practice that respond well to physiotherapy. Over the last several years, I’ve seen commonality between clients with certain pain presentations. This makes it very clear as to what treatments may work best in decreasing your pain and returning to the activities you love participating in. There are slight variations between each client but most of the guiding principles are similar. Just a reminder, this doesn’t substitute a proper assessment and treatment plan, but it may shed light on whether physiotherapy would be right for you.
The following are questions a physiotherapist would ask you when taking a thorough history. This presentation is usually more common in females aged 25-39 years old.
How does it feel?
In many cases of lower back presentations, there is one side that is more dominant. You can either have left or right sided pain. I’ve also seen pain that is equally uncomfortable across the back, however as things progress it can become more intense on one side.
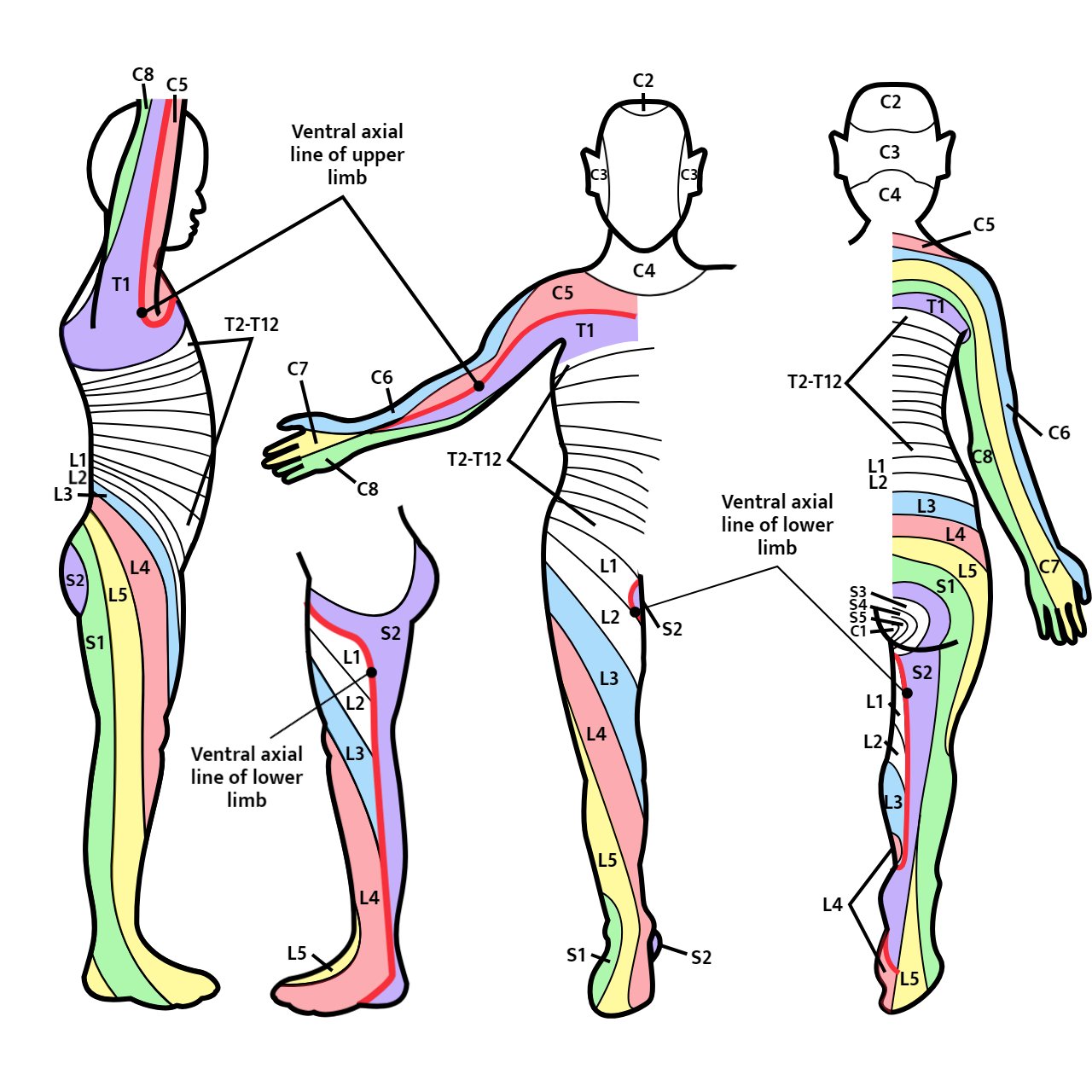
Lower back pain can either be constant or intermittent in nature. You could have tingling and/or numbness down one leg, and it’s usually on the same side as your back pain. Tingling or numbness can happen in just one area of the leg, or it can run from your back to your foot in a very distinct pattern. These patterns are called dermatomes and are sensory distributions for a specific nerve from your back. Based on where the symptoms are, this can help pinpoint the exact level in your spine you are having an issue.
It's helpful to hear what others have to say about what it feels like when they experience this numbness or tingling. Here are some descriptions my clients have expressed when dealing with nerve related pain:
Dermatomes of the arms of legs
“Something just doesn’t feel right”
“I feel like I have someone else’s leg”
“My leg doesn’t feel like it’s there”
“It feels numb-ish”
“My leg feels swollen”
“It feels like I’m wearing a tight sock or shoe on my foot”
What makes it worse?
Walking or standing for long periods increases the leg symptoms of tingling and numbness. Bending backwards or doing the cobra can also make your back and leg symptoms worse. Other positions that might be uncomfortable are sitting upright with a nice curve in your back. You may find strangely enough that slouching improves your back and leg pain. If you have children, carrying them on your hip can be very aggravating. If you work in manual labour jobs, carrying something heavy in front while walking may also worsen your symptoms. Massage in the areas of soreness may worsen your symptoms, but may also temporarily or even permanently improve your symptoms.
What makes it feel better?
Sitting, lying down with knees bent, or anything that puts your spine in a bit of flexion. Positions like child’s pose or being in the fetal position relieve pain temporarily. Sometimes anti-inflammatories, like naproxen or ibuprofen, can provide temporary relief as well. Depending on the issue, massage can certainly improve symptoms, but it is important to understand what the injury is before applying pressure as there could be a risk of worsening of symptoms.
What do you do for work?
I find that a lot of female elementary school teachers who work with younger kids will need to stoop, bend forward, and sit in small chairs when working with their students. Sitting on the floor can be extremely uncomfortable for some of my clients because of the stress it can put on their back and hip. Other times, especially at the start of the school year, moving boxes of classroom supplies can cause an increase of lower back pain. This results in a very sore lower back by the end of the day and not enough gas in the tank for hobbies, recreational sports, or for their own family at home.
Another common group who sustains this injury are female nurses who have to complete a lot of transfers or boosts for their clients. Their job is tricky because their lifting mechanics will not be ideal based on their situation. Sometimes the bed their patient is in doesn’t move up or down. In other circumstances, they are rushed for time. Currently there is a shortage of staff in rest homes and hospitals, including personal support workers (PSW), registered practical nurses (RPN) and registered nurses (RN). The number of people available for a transfer is limited, which can result in more injuries. In many other cases, patients can either be bariatric, which can increase the load on a nurse’s back, or they can be resistive because of a disability, increasing the chances of unsafe transfers and more muscles activated to hold patients safely.
How old are you?
Most commonly younger individuals between the ages of 25-39 years old. Some people laugh when I say young because they certainly don’t feel young with back injuries. I’ve heard people say, “it goes downhill from (fill in your age)”. Most times, age itself is not the strongest predictive factor, as this injury is not strictly limited to this age range, and can vary from person to person.
When did your injury start?
It can range from days to years, but more recently many of my clients have reported a history of 6-8 months. You may have had an on and off history of lower back pain. Many people disregard an ache in the back because it doesn’t stop them from continuing their daily routine. They may be slightly concerned, but not enough to investigate it or seek professional help. The aches or pains in your back that are not a current concern would recur throughout the year until it either becomes more intense or constant. It begins to impede your daily routine and you may start noticing tingling, numbness or weakness down your leg. At that point, people begin searching for physiotherapy, chiropractic, and massage for pain relief. I often meet people after they’ve seen 1-3 different health care practitioners.
Have you had any previous surgeries or trauma?
The common vein with this presentation is childbirth or a c-section within the last year. However sometimes I’ve had patients dealing with this for more than a year who have also had a complicated pregnancy years ago.
Other times it could be a hernia repair, or other surgeries that require you to cut through the abdominal wall. This can result in weakening of the muscles in the front of your belly contributing to back pain.
Another common traumatic event is a motor vehicle accident. Not experiencing any immediate pain, you may have been involved in a car accident but didn’t notice any problems and carried on with regular life. Slowly over time, you may have noticed an increase in lower back pain. You may have forgotten about the motor vehicle accident and attributed it to old age or an even older sport injury. Car accident injuries can often come up months later unbeknownst to the passenger or driver. It’s important to get a checkup from a physiotherapist who can provide insight on anything that could be wrong after the injury.
Okay, so this sounds like me – what do I do?
You can try adopting the positions that provide the most relief, resting from your regular recreational activities, and avoiding the most aggravating positions. If you need to stay active you can continue your activity but stop before symptoms worsen. Ice or heat may also provide relief; the research supports whatever feels best at the time (although ice can hinder the healing process – read about it here). Otherwise, if things don’t dramatically improve after 2 weeks, it may be time to see a physiotherapist. Physiotherapists at Break Free are skilled in finding patterns during your daily life to ensure that your healing process is smoother. It won’t be perfect as there are multiple factors involved, but by listening to your story and understanding your lifestyle, we can provide recommendations to help you return to doing the things you love. That could be playing with your kids, working out, running, or any other recreational sport.
I wish I could provide the “Top 3 Exercises to Fix Back Pain”, but here at Break Free we are all about diagnostic accuracy. That means providing the exact exercises for your condition. There is no “1 exercise fits all” approach, as your injury is unique and your body is different from others. There are similarities in anatomy and structure, but we ultimately want to listen to your story and find the best treatment based on your presentation.
How long will this take to heal with physiotherapy?
In the case of physiotherapy, the earlier you can treat an injury, the higher your chances of success are. The type of treatment has to match what injury you may be suffering from. Also, the time elapsed is a large factor in how long it will take to heal. The longer it has been since the injury, the longer it may take to heal. Most medical textbooks will say that greater than 3 months is chronic. In most cases, if you can begin treatment prior to that, your outcomes may be better. Age can also be a factor, as with age, your ability to heal is slower than someone who is younger.
We love helping people get to back to activity. It’s our joy to see people walk out the door with tools to maintain their health and live well. If you are interested in learning more, book now with one of our movement specialists today! We’d love to meet you and hear your story.